Cholesterol is a waxy substance that's found in the fats (lipids) in your blood. While your body needs cholesterol to continue building healthy cells, having high cholesterol can increase your risk of heart disease.
When you have high cholesterol, you may develop fatty deposits in your blood vessels. Eventually, these deposits make it difficult for enough blood to flow through your arteries. Your heart may not get as much oxygen-rich blood as it needs, which increases the risk of a heart attack. Decreased blood flow to your brain can cause a stroke.
High cholesterol can be inherited, but it's often the result of unhealthy lifestyle choices, and thus preventable and treatable. A healthy diet, regular exercise and sometimes medication can go a long way toward reducing high cholesterol.
Symptoms
High cholesterol has no symptoms. A blood test is the only way to detect high cholesterol.
When to see a doctor
Ask your doctor if you should have a cholesterol test. Recommendations for the age of first screening vary. Retesting is usually performed every five years.If your test results aren't within desirable ranges, your doctor may recommend more frequent measurements. Your doctor may also suggest you have more frequent tests if you have a family history of high cholesterol, heart disease or other risk factors, such as smoking, diabetes or high blood pressure.
Causes
Cholesterol is carried through your blood, attached to proteins. This combination of proteins and cholesterol is called a lipoprotein. You may have heard of different types of cholesterol, based on what type of cholesterol the lipoprotein carries. They are:
- Low-density lipoprotein (LDL). LDL, or "bad," cholesterol transports cholesterol particles throughout your body. LDL cholesterol builds up in the walls of your arteries, making them hard and narrow.
- High-density lipoprotein (HDL). HDL, or "good," cholesterol picks up excess cholesterol and takes it back to your liver.
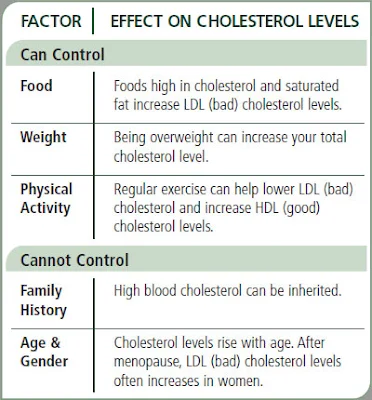
Factors within your control — such as inactivity, obesity and an unhealthy diet — contribute to high LDL cholesterol and low HDL cholesterol. Factors beyond your control may play a role, too. For example, your genetic makeup may keep cells from removing LDL cholesterol from your blood efficiently or cause your liver to produce too much cholesterol.
Risk factors
- Poor diet. Eating saturated fat, found in animal products, and trans fats, found in some commercially baked cookies and crackers, can raise your cholesterol level. Foods that are high in cholesterol, such as red meat and full-fat dairy products, will also increase your total cholesterol.
- Obesity. Having a body mass index (BMI) of 30 or greater puts you at risk of high cholesterol.
- Large waist circumference. Your risk increases if you are a man with a waist circumference of at least 40 inches (102 centimeters) or a woman with a waist circumference of at least 35 inches (89 centimeters).
- Lack of exercise. Exercise helps boost your body's HDL, or "good," cholesterol while increasing the size of the particles that make up your LDL, or "bad," cholesterol, which makes it less harmful.
- Smoking. Cigarette smoking damages the walls of your blood vessels, making them likely to accumulate fatty deposits. Smoking may also lower your level of HDL, or "good," cholesterol.
- Diabetes. High blood sugar contributes to higher LDL cholesterol and lower HDL cholesterol. High blood sugar also damages the lining of your arteries.
Complications
High cholesterol can cause atherosclerosis, a dangerous accumulation of cholesterol and other deposits on the walls of your arteries. These deposits (plaques) can reduce blood flow through your arteries, which can cause complications, such as:
- Chest pain. If the arteries that supply your heart with blood (coronary arteries) are affected, you may have chest pain (angina) and other symptoms of coronary artery disease.
- Heart attack. If plaques tear or rupture, a blood clot may form at the plaque-rupture site — blocking the flow of blood or breaking free and plugging an artery downstream. If blood flow to part of your heart stops, you'll have a heart attack.
- Stroke. Similar to a heart attack, if blood flow to part of your brain is blocked by a blood clot, a stroke occurs.
Diagnosis
A blood test to check cholesterol levels — called a lipid panel or lipid profile — typically reports:
For the most accurate measurements, don't eat or drink anything (other than water) for nine to 12 hours before the blood sample is taken.
- Total cholesterol
- LDL cholesterol
- HDL cholesterol
- Triglycerides — a type of fat in the blood
For the most accurate measurements, don't eat or drink anything (other than water) for nine to 12 hours before the blood sample is taken.
Treatment
Lifestyle changes such as exercising and eating a healthy
diet are the first line of defense against high cholesterol. But, if
you've made these important lifestyle changes and your cholesterol
levels remain high, your doctor may recommend medication.
The specific choice of medication or combination of medications depends on various factors, including your individual risk factors, your age, your current health and possible side effects. Common choices include:
If you choose to take cholesterol-lowering supplements, remember the importance of a healthy lifestyle. If your doctor prescribes medication to reduce your cholesterol, take it as directed. Make sure your doctor knows which supplements you're taking as well.
The specific choice of medication or combination of medications depends on various factors, including your individual risk factors, your age, your current health and possible side effects. Common choices include:
- Statins. Statins block a substance your liver needs to make cholesterol. This causes your liver to remove cholesterol from your blood. Statins may also help your body reabsorb cholesterol from built-up deposits on your artery walls, potentially reversing coronary artery disease. Choices include atorvastatin (Lipitor), fluvastatin (Lescol), lovastatin (Altoprev), pitavastatin (Livalo), pravastatin (Pravachol), rosuvastatin (Crestor) and simvastatin (Zocor).
- Bile-acid-binding resins. Your liver uses cholesterol to make bile acids, a substance needed for digestion. The medications cholestyramine (Prevalite), colesevelam (Welchol) and colestipol (Colestid) lower cholesterol indirectly by binding to bile acids. This prompts your liver to use excess cholesterol to make more bile acids, which reduces the level of cholesterol in your blood.
- Cholesterol absorption inhibitors. Your small intestine absorbs the cholesterol from your diet and releases it into your bloodstream. The drug ezetimibe (Zetia) helps reduce blood cholesterol by limiting the absorption of dietary cholesterol. Ezetimibe can be used in combination with a statin drug.
- Injectable medications. A new class of drugs can help the liver absorb more LDL cholesterol — which lowers the amount of cholesterol circulating in your blood. Alirocumab (Praluent) and evolocumab (Repatha) may be used for people who have a genetic condition that causes very high levels of LDL or in people with a history of coronary disease who have intolerance to statins or other cholesterol medications.
Medications for high triglycerides
If you also have high triglycerides, your doctor may prescribe:
- Fibrates. The medications fenofibrate (TriCor, Fenoglide, others) and gemfibrozil (Lopid) decrease triglycerides by reducing your liver's production of very-low-density lipoprotein (VLDL) cholesterol and by speeding up the removal of triglycerides from your blood. VLDL cholesterol contains mostly triglycerides.
- Niacin. Niacin decreases triglycerides by limiting your liver's ability to produce LDL and VLDL cholesterol. But niacin doesn't provide any additional benefit than using statins alone. Niacin has also been linked to liver damage and stroke, so most doctors now recommend it only for people who can't take statins.
- Omega-3 fatty acid supplements. Omega-3 fatty acid supplements can help lower your triglycerides. They are available by prescription or over-the-counter. If you choose to take over-the-counter supplements, get your doctor's OK first. Omega-3 fatty acid supplements could affect other medications you're taking.
Tolerance varies
Tolerance of medications varies from person to person. The common side effects are muscle pains, stomach pain, constipation, nausea and diarrhea. If you decide to take cholesterol medication, your doctor may recommend liver function tests to monitor the medication's effect on your liver.Children and cholesterol treatment
Diet and exercise are the best initial treatment for children age 2 and older who have high cholesterol or who are obese. Children age 10 and older might be prescribed cholesterol-lowering drugs, such as statins, if they have extremely high cholesterol levels.Alternative medicine
Few natural products have been proven to reduce cholesterol, but some might be helpful. With your doctor's OK, consider these cholesterol-lowering supplements and products:- Barley
- Beta-sitosterol (found in oral supplements and some margarines, such as Promise Activ)
- Blond psyllium (found in seed husk and products such as Metamucil)
- Oat bran (found in oatmeal and whole oats)
- Sitostanol (found in oral supplements and some margarines, such as Benecol)
If you choose to take cholesterol-lowering supplements, remember the importance of a healthy lifestyle. If your doctor prescribes medication to reduce your cholesterol, take it as directed. Make sure your doctor knows which supplements you're taking as well.













No comments:
Post a Comment